Hit enter to search or Esc to close
Case Study
Providing insight to the elective challenge

The elective challenge
Waiting times for elective care have been under pressure for a long time, but COVID-19 caused a dramatic escalation. At the height of the pandemic, many routine and elective procedures were paused to prioritise emergency care and respond to the urgent needs of patients with COVID-19. As a result, a substantial backlog built accumulated. By 2024, the elective waiting list in England had grown to over 7.5 million with nearly 1 in 8 of the UK population on an elective waiting list.
To meet this challenge the government and NHS England have launched several initiatives.
- Elective recovery plans: targeted investment in staff, facilities, and technology, including surgical hubs and community diagnostic centres, to increase capacity and efficiency.
- Use of the independent sector: collaborations with private healthcare providers to increase the volume of elective procedures.
- Prioritisation and triage: systems to ensure those in greatest clinical need or who have been waiting longest are treated first.
- Digital innovation: expansion of virtual consultations and digital tools to streamline patient pathways and reduce administrative delays.
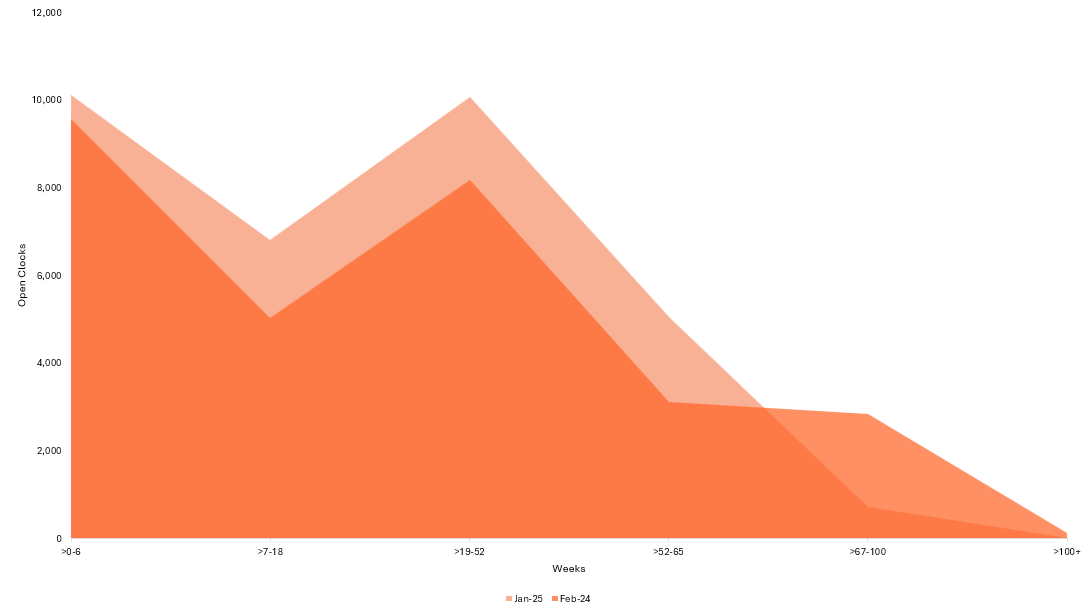
However, the situation remains challenging. Although the number of people waiting the longest has reduced, the profile of people waiting has shifted and the overall list size remains largely unchanged.
In January 2025, the NHS published a new ambition to reform elective services and increase the percentage of patients treated within 18 weeks to 65% by March 2026, with a further increase to 92% by March 2029.
To meet this challenge, one large multi-site acute teaching trust asked Newton to help by bringing an innovative dynamic flow-based approach to the development of their recovery plan; a task they knew would be incredibly challenging. Newton’s rigorous, data-led approach has provided the trust with the insight they need to meet the challenge.
Working together to understand the challenge
Newton, alongside the trust’s operational, clinical and BI teams were able to provide a level of insight that enabled the trust to understand:
- the areas with the greatest opportunity to improve and how to access them – by speciality, point in the pathway, operational planning guidance, and operational delivery lever
- the relative potential for each opportunity to impact performance for prioritisation
- the requirement for dynamic solutions and recognise the knock-on impact of improvements across the pathway
and to forecast required performance trajectory including clock start / stop requirements to meet targets, highlighting delivery risks for further consideration.
We showed that:
Over 55% of people with open clocks were waiting for a first outpatient appointment, and over 75% of patients have their clocks stopped in their first outpatient appointment.
Up to 40% of patients would have benefitted from a ‘straight to test’ pathway, improving patient experience and RTT performance.
Bringing a flow-based approach to elective recovery
The Newton team were able to bring the sophisticated, dynamic flow-based approaches that have been so critical to solving Urgent and Emergency Care (UEC) flow across systems and apply the same technology, processes and predictive based thinking to elective recovery. This involved:
Pathway Deep Dives – operational
With agreed speciality and Points of Delivery (POD) areas, Newton worked alongside data validators to review cases and processes to further understand patient pathways and the opportunities to improve elective care performance.
Static Data Analysis
Combining publicly available and trust provided data, to analyse how the trust’s performance compared nationally and identified focus areas within the trust.
Dynamic Analysis
With the basis of data analysis and case studies examined, a dive further into the data to identify the specific improvements that could be implemented. Creating a dynamic view of how the waitlist is changing over time.
Scenario Modelling
Utilising the patient pathways identified from the case studies and the dynamic analysis, modelling how the suggested improvements would drive better 18-week performance and simulating how this would impact waiting lists at different parts of the patient pathway.

Providing actionable insights
Through the deployment of technology and approaches that have been so critical to solving complex UEC flow optimisations and applying them alongside a deep understanding of elective care, Newton were able to surface actionable insight for the clinical, operational and leadership teams. Allowing the trust to build an optimised recovery plan that will dramatically reduce the numbers waiting for care over the next three years and contribute to achieving the 65% and 92% targets by 2029.
We are really excited to be able to wrap this insight alongside Newton’s fee guarantee model to make a meaningful contribution to helping NHS trusts reduce the numbers of people waiting for care, enabling them to deliver better outcomes at a lower cost.